Should You Get Genetic Testing To Gauge Your Breast Cancer Risk? Expert Weighs In - Exclusive
You've probably heard of genetic testing for breast cancer or maybe even read the letters BRCA in an article somewhere, but how do you know if it's something you should personally look into? Most women know to perform at-home exams and regularly get mammograms to check for breast cancer, but did you know that only around 25 percent of women who have been diagnosed with breast cancer have any genetic testing done? This lack of testing can have negative health outcomes for women that might need certain kinds of treatments depending on the genetic makeup of their cancer. Not to mention, while there has been an increase in preventative BRCA screening since 2007, the number of women pursuing this genetic screening is not nearly enough (data suggests it's less than 1 percent).
Despite the fact this testing can be absolutely vital for women, cost and a general lack of education have impacted how many women actually utilize genetic testing. Beyond changing how you might choose to handle a breast cancer diagnosis, a confirmed genetic mutation can also change your preventative screening needs. For example, women with confirmed BRCA1 or BRCA2 inherited gene mutations need breast cancer screenings much more frequently and also starting at a much younger age than those who do not have the mutation. Women.com exclusively connected with Dr. Gail Lebovic, oncoplastic surgeon, breast cancer specialist, and former President of the American Society of Breast Disease to learn about BRCA mutation testing and when it could be something worth discussing with your doctor.
What exactly is BRCA testing
Breast cancer is not only the second most diagnosed cancer in the U.S., it is also the second leading cause of cancer-related mortality. Some of these breast cancers have a genetic (i.e. inherited) component. Researchers have discovered that genetic mutations in the BRCA1 and BRCA2 genes have a strong correlation to the development of certain types of breast cancers. Dr. Lebovic explained that the BRCA mutation "indicates that there is a mutation within a specific genetic coding sequence which is inherited." From this research, doctors developed genetic screenings to look at these specific genes in order to gauge whether a person has a BRCA1/BRCA2 mutation or not. It is also important to note that BRCA gene mutations can similarly correlate to higher risks of ovarian cancer.
Research estimates that women with the BRCA1 mutation have a 55 to 72 percent chance and women with a BRCA2 have a 45 to 69 percent chance of developing breast cancer compared to a 13 percent chance of breast cancer among the general population. Blood relatives of those with these BRCA mutations can have up to a 50 percent chance of having the same mutations, which makes this genetic testing even more important for families with a known history of breast cancer. With that being said, most breast cancers are not BRCA mutations so it's important to realize that the BRCA testing can't give you any specific guarantees about your potential to develop breast cancer.
Who should get tested
If you are someone with no family history of breast cancer, chances are you don't have an inherited BRCA mutation to worry about. Dr. Lebovic exclusively told us, "Since these mutations only account for 10 to 15 percent of all breast cancers, very few women actually need to have genetic testing. Usually, when a primary care physician or OB/GYN has a patient who has a number of first-degree (for example Mother, Sister, Aunt) family members that have had breast cancer at a relatively young age (under 60) then we would likely order genetic testing."
It's important to remember that harmful BRCA variants only affect about 0.2 percent of the U.S. population. With that being said, for those with a known family history of breast cancer (or those without family health history knowledge for any reason) speaking to your doctor about genetics testing could be something worth pursuing. Having more information about your genetic makeup can ultimately help you prepare for the future. Knowledge is power.
How does testing work?
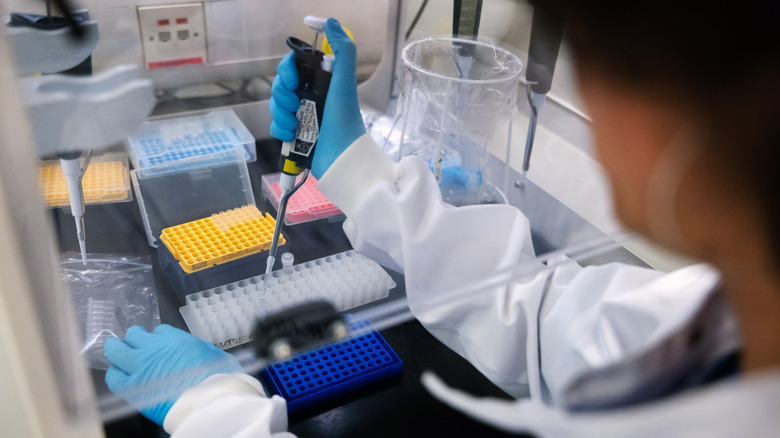
You might be wondering just how invasive this kind of genetic testing is. The good news is that BRCA1/BRCA2 mutations are normally tested using a simple blood, saliva, or cheek swab test. One of the biggest hurdles you might face is actually the cost and/or insurance hurdles associated with getting genetic testing. Researchers have found gaps in varying insurance coverage for both genetic testing and subsequent recommended interventions/treatments which can make it difficult for people to get BRCA testing in the first place.
Some doctors might also refer you to a genetic counselor for testing. These counselors can best determine if and what testing is right for you. In our exclusive interview, Dr. Lebovic emphasized, "It's very important to meet with a skilled genetic counselor to discuss the risk of developing breast cancer and/or ovarian cancers because these mutations are associated it these two types of cancers." Genetic counselors offer information about certain genetic conditions based on your and/or your family's medical health history. These counselors can help determine if you'd be a good candidate for further genetic testing and what exactly to test for. Genetics counseling can be important at various stages in your life from pregnancy concerns like fertility to having young children tested for inherited defects and disabilities.
What can BRCA testing be used for
While BRCA 1/BRCA2 gene mutations can tell you if you have a higher risk of getting breast and ovarian cancer, it is by no means a guarantee or affirmative diagnosis. Dr. Lebovic explained in our exclusive interview that this testing can leave people with a lot to consider: "Decision-making is complex and must take into account many factors such as age, family history, hormonal history, breast density, and others. Certainly, psychosocial issues are also critically important to discuss and so we encourage each and every woman with a known mutation to take the time and critically analyze their decision process."
Your BRCA mutation results can ultimately help you determine the frequency of your future screenings and can even potentially lead to certain preventive care options. If you have a confirmed BRCA mutation, Dr. Lebovic emphasized that "the chances of developing cancer are greater but they are not 100 percent. This is a very important factor to remember when considering how aggressive to be when it comes to [preventative] surgery."
For those without a BRCA1/BRCA2 mutation, it's important to remember that your risk for breast cancer still exists. Many factors can still ultimately contribute to your risk of developing breast cancer including smoking, obesity, estrogen hormone use, and even alcohol consumption. Remember that a negative BRCA mutation test does not guarantee a breast cancer-free life and that you should always stay up-to-date with your screenings.
What do I do with my results?
While the general recommendation for those with confirmed BRCA mutations is regular and more frequent screenings including mammograms, MRIs, and ultrasounds, not all women go this route. "Some women are not comfortable with the "watch and see" approach, and they choose surgery as the solution for removing the breast tissue and ovaries," Dr. Lebovic explained in our exclusive interview.
Celebrities like Christina Applegate and Angelina Jolie both famously underwent preventative surgeries (Applegate opting for a double mastectomy despite her breast cancer being in one breast, and Jolie opting for a fully preventative double mastectomy) when they discovered they had the BRCA1 gene mutation. Research shows that preventative mastectomies can reduce your chances of developing breast cancer by 90 percent or more and that the rate of women opting for them is increasing.
For those without a BRCA mutation, Dr. Lebovic emphasized that you should still take your at-home breast exams seriously, because "the vast majority of breast cancers are not linked to a genetic mutation." She highlighted that women are recommended to begin their yearly mammogram screening, regardless of BRCA or family history, starting at age 40, "Routine mammography screening and/or ultrasound screening every year are the gold standard for the majority of women." As always, it is best to discuss your screening and treatment options with your doctor to determine what will work best for your care.